What Is Functional Medicine?
At CCFM, we are proud to offer a different form of healthcare – functional medicine – that is uniquely poised to not only address and reverse chronic conditions but improve long-term health and well-being.
Conventional medicine has its strengths, particularly in the areas of emergency medicine and surgery. However, it falls short in treating chronic illnesses, particularly complex chronic conditions.
The statistics on chronic diseases are in, and they are alarming. According to recent CDC estimates, six out of every ten American adults have a chronic disease, and four in ten have two or more chronic diseases.1 Unfortunately, the conventional medical model has little to offer in treating these conditions beyond watchful waiting, medication, and surgery. In the case of complex chronic illnesses, such as autoimmune diseases, chronic gastrointestinal illnesses, or Lyme disease, conventional medicine has even less to offer. Conventional medicine frequently tries to prune back the final manifestations of disease by trying to control or suppress symptoms without asking why those symptoms are occurring in the first place. When it comes to treating chronic illnesses, we need to think outside the box of conventional medicine and look for the root cause of illness and intervene as far down the chain as possible, at the root cause.
What is Functional Medicine?
Functional medicine is a holistic, collaborative approach to healthcare that places the patient front and center. Rather than only managing disease, functional medicine seeks to address the root causes of poor health.
The discipline of functional medicine was founded by Dr. Jeffrey Bland, a biochemist, in 1990. Dr. Bland recognized that our "pill for an ill" conventional medical system was not effectively addressing the underlying causes of disease, and saw a need for taking a more comprehensive, systems-biology approach to the prevention and management of chronic disease. The result was the establishment of functional medicine, a distinct approach to healthcare that is science-based, cross-disciplinary, and considers all aspects of health when caring for the patient. In subsequent years, Dr. Mark Hyman and The Institute for Functional Medicine furthered the development of this growing field.
The differences between conventional and functional medical care can be compared to managing a garden. In your garden, which represents your body, you need to feed the soil, keep pests away, and control weeds, which represent factors that contribute to chronic disease. The conventional approach to (disease) management is to spray the pests and weeds with pesticides or herbicides or to mow the weeds down with a weed whacker. While these strategies eliminate the pests and weeds over the short-term, they sometimes come back with a vengeance!
Furthermore, the organism, soil, and garden are weakened and damaged by the toxins. On the other hand, functional medicine works to strengthen the entire system, improve the terrain itself, keep pests away holistically, and pull the weeds of disease up by the roots. We work to promote a healthier garden, and a healthier you, for the long-term.
The growth of functional medicine hasn’t come without pushback from the conventional medical community. However, the scientific community is slowly recognizing the profound benefits of this healthcare approach. In fact, a recent study published in the prestigious Journal of the American Medical Association reports that the functional medicine model of care may have “the ability to improve global health in patients.”2 In coming years, we will likely see continued research into this model corroborating the positive experiences of countless functional medicine providers and patients.
The Pillars of Functional Medicine
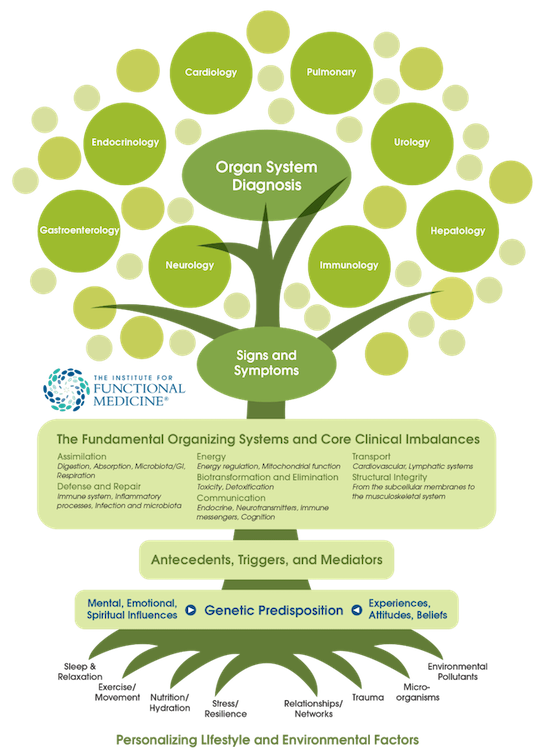
Conventional medicine views the body as a set of disparate parts and systems; this is evidenced by the fact that we have separate doctors or specialists for literally every part of the body! In the conventional medical model, you must visit a gastroenterologist for gut issues, a cardiologist for cardiovascular concerns, an endocrinologist for hormone problems, a dermatologist for skin troubles, etc. To make matters worse, conventional specialists are siloed and often provide conflicting information and do not communicate with one another, making the recovery process complicated and frustrating for the patient.
Conversely, functional medicine is a holistic approach that looks at the body as a complex, interconnected set of systems, rather than as individual body parts. We also understand that every person is unique and that treatments must be individualized, a concept we call “biochemical individuality.”
Addressing the Roots of Chronic Disease
As you learned with the garden metaphor above, functional medicine seeks to address the root causes of disease as far down the causal chain as possible, rather than merely managing symptoms with drugs or intervening with surgery.
Some of the roots of chronic disease that functional medicine addresses include:
Gut dysfunction and gut microbiome imbalances
Over 70% of our immune system is found in the digestive tract and there is a strong connection between gut dysfunction and many, if not most, illnesses.3,4 With every patient we see, we perform comprehensive testing to look for common issues such as yeast overgrowth, dysbiosis (an imbalance between healthy and unhealthy strains of bacteria), small intestinal bacterial overgrowth (SIBO), and gut inflammation. You might think that gut dysfunction would always manifest as digestive symptoms, but that is not always the case. While many of our patients do have GI issues that need to be addressed, impaired gut function can also manifest as skin rashes, anxiety/depression, cognitive impairment, sleep disruption, joint pain, or fatigue, among many other things. No matter what the symptoms, we always look at the gut as a starting place for intervention.
Autoimmune activation
Our immune system is amazingly complex and elegant. Unfortunately, we are witnessing a meteoric rise in autoimmune conditions such as Rheumatoid Arthritis, Hashimoto’s thyroid disease, Sjogren’s syndrome, Ulcerative Colitis or Crohn’s disease, and more. Conventional medicine has limited treatment options for autoimmune diseases. Doctors often use expensive or poorly tolerated medications to turn off or control the overactive immune response and reduce inflammation. Unfortunately, this rarely addresses the main question in autoimmune cases: “what is causing the immune system overactivation?” At CCFM, this is our starting place. From there, we work to identify and treat root causes to enable the immune system to reset and calm down. With this approach, we help alleviate the associated symptoms. Gut dysfunction and chronic infections are significant triggers for autoimmune activation, and these must be addressed for the body to reset and heal.5,6
Hormone imbalances
Our body’s hormonal systems all operate in a delicate balance and communication with each other. We carefully investigate the function of the various systems from the thyroid, adrenal, and sex hormones like estrogen, progesterone, and testosterone, to metabolic hormones like insulin, leptin, and adiponectin. It is not uncommon for us to see symptoms and lab markers showing adrenal dysregulation, estrogen dominance, or low thyroid function. We combine lifestyle and behavior modification to normalize hormones. We also incorporate nutritional interventions, dietary supplements, vitamins, and nutrients to help the body's hormonal systems regain their function. As appropriate, and in careful discussion with each individual, we also recommend bio-identical hormone support.
Chronic infections
As microbiologist Dr. Justin Sonnnenberg of Stanford University has said, humans are essentially elaborate transport mechanisms for other microbes, which we carry on and in our bodies in staggering numbers.7 While numerous microorganisms are vital for our health, many can cause, trigger, or exacerbate illnesses. Many pathogens can exist as persistent infections or be reactivated when our bodies become imbalanced, causing various symptoms. These might include tickborne illnesses like Lyme disease and coinfections, Epstein-Barr (EBV) or other viruses, Chlamydia, Mycoplasma, and chronic inflammatory response syndrome (or mold illness). Identifying chronic infections and their effects on your health can be complicated and nuanced, but is critical to provide targeted treatment to get you better.
Inflammation
Inflammation is a key driver of many, if not all, chronic diseases, including diabetes, coronary heart disease, Alzheimer’s disease, and chronic fatigue, to name but a few.8 Numerous factors contribute to inflammation. However, we can modulate inflammation through interventions such as gut-healing protocols, treatment of chronic infections, meditation, exercise, and sleep, and more. Our goal is to discover where the hidden fire is and put it out, address why the fire started in the first place, and clean up the collateral damage.
Environmental exposures
While many people think of genetics as fixed and unchangeable, only a tiny minority of illnesses are determined fully by your genetic makeup. Rather, it is your diet and lifestyle choices and environmental exposures that are most influential in determining your health status. The process through which environmental cues change the expression of your genes and impact your health, without altering your underlying genetic code, is called “epigenetics.”12 While it may sound complicated, the important take-home message is that your genes are not always in control. You are!
Genetics and epigenetics
While many people think of genetics as fixed and unchangeable, only a very small minority of illnesses are determined fully by your genetic makeup. In fact, your lifestyle choices, environmental exposures, and internal body environment constantly communicate with your genes, switching genes on and off, changing which proteins and enzymes are produced, and how your body functions. You may have heard the phrase “genetics load the gun, but the environment pulls the trigger.” Another way of saying this is the more recent aphorism, “your zip code is more important than your genetic code.” Epigenetics is the growing area of science that studies how our genes are affected by what we are exposed to. You can think about it as a type of biochemical process or tag that switches genes on or off. While it may sound complicated, the important take-home message is that your genes are not always in control. You are!
Nutrition and food as medicine
It is often said that food can either be medicine or poison. We believe that food is the foundation of good health, and we use nutritional prescriptions and interventions with every patient we work with. Unfortunately, we live in a time where our foods are increasingly toxic and nutritionally depleted. There are many “food-like” products that people consume on a daily basis, most of which are highly processed and create inflammation in our bodies. We prioritize a nutritional approach that provides nutrient-dense foods, minimizes inflammation, and helps your body systems function optimally.
Stress and allostatic load
Allostatic load is "the wear and tear on the body" which accumulates as an individual is exposed to repeated or chronic stress.13 Chronic stress and a high allostatic load can significantly affect all aspects of health, including your mood and brain function, resulting in accelerated aging, inflammation, hormone disruption, immune dysregulation, and much more. Many factors act as stressors for your body, including hidden infections, poor sleep, inadequate movement, or an unhealthy diet. Furthermore, stressful experiences stack up over time, further depleting the body. Our goal is to identify current and past stressors, modify or eliminate them to decrease the overall load experienced by your system and to help you process and heal your brain and nervous system to get you better.
Sleep
In his book Why We Sleep, Dr. Matthew Walker said it simply, “The shorter your sleep, the shorter your lifespan.” As a global society, we are in the midst of an epidemic of inadequate and poor quality sleep. Many people do not realize that poor sleep contributes to increased rates of cardiovascular diseases, metabolic diseases like diabetes, weight gain, cancer, anxiety and depression, suicide, and impaired immunity. Sleep is needed for our body to repair and rejuvenate itself; without it, our health will decline. At CCFM, we work closely with all patients to optimize sleep. We provide comprehensive testing to identify underlying imbalances that may be triggering poor sleep, coaches trained in the science of behavior change, advanced wearable technology (such as the Oura ring) to provide sleep data, proven lifestyle hacks, and supplements help you sleep better, feel rested, and function to your full potential.
Movement and exercise
What is standing in the way of getting more exercise? Most people report either a shortage of time or energy as barriers to making exercise a regular habit. We all know that exercise/movement helps with weight loss and/or weight maintenance, but it also is linked to improvements in the gut microbiome and improvement in mental health symptoms like anxiety and depression. Our bodies were designed to move, and healthy movement is an important foundation for overall health. A large study involving over 100,000 U.S. adults found that those who sat for more than six hours a day had up to a 40 percent greater risk of death over the next 15 years than those who sat for less than three hours a day. We strive to help our patients incorporate more exercise, active movement, and “non-exercise” physical activity into their day.
Respecting the Contribution of Diet and Lifestyle to Health
Conventional medicine frequently gives lip service to the importance of nutrition and lifestyle in the prevention and management of chronic disease but offers very little in the way of ongoing, evidence-based care in these areas. On the other hand, functional medicine thoroughly considers the contribution of lifestyle factors, including diet, sleep, exercise, and stress to physical health, and provides you with the tools and support to optimize these areas of your life. At CCFM, we often recommend lifestyle changes and therapeutic diets as part of the treatment plan because these factors have such a significant influence on health and healing.
We know from personal experience and decades of patient care experience that making successful health behavior change is hard. This drives our passion for building a world-class team to help you succeed.
Functional Medicine is Patient-Centered
In the conventional medical model, doctors spend a mere 15 minutes with patients in a single appointment.14 This is barely enough time to greet the patient, let alone get to the root of the patient’s health problems, and offer helpful solutions! The functional medicine doctor, on the other hand, will frequently spend an hour or more thoroughly getting to know the patient.
Understanding what led to symptoms/disease takes time. At CCFM, we know that it’s imperative to spend time going through a patient’s history. We want to know everything that has happened to you from when you were in your mother’s womb until the moment we meet. By gathering a comprehensive medical history, we can often connect the dots and begin the necessary investigation and detective work.
At CCFM, we take a comprehensive care-team approach to help you recover. Our team includes a physician, a midlevel provider (NP/PA), a nutritionist, a health coach, and compassionate admin staff. We use a variety of comprehensive tests that allow for a deep dive into inflammatory markers, gut health, adrenal/hormone imbalance, nutrient deficiencies, mold markers, and hidden infections such as Lyme, coinfections, and others.
We also recognize the mental and emotional burden you can experience when you don’t necessarily look “sick” on the outside. Many of our patients have been disappointed in the past by their healthcare encounters, or they feel like they were ignored or written off by their providers. We understand that feeling unwell doesn’t always have external manifestations and that many suffer from invisible illnesses that leave them unseen by the healthcare system, and family, friends, and society in general. Our team is here to support you every step of the way on your journey back to health.
Functional Medicine is Individualized
The root causes of illness differ from one person to the next based on diet and lifestyle variables, genetics, biochemical individuality, and environmental exposures. Functional medicine recognizes that there is no single cause of any given disease, and there cannot be a one-size-fits-all approach to chronic disease treatment. Instead, at CCFM, our functional medicine approach treats each patient as an individual by first collecting a detailed health history and laboratory testing, and leveraging this information to direct the development of a personalized treatment plan.
The personalized treatment plan developed by your functional medicine team may include:
- Nutrition prescriptions
- Lifestyle recommendations that address sleep, exercise, and stress management
- Treatments for supporting gut health and targeting gut infections
- Hormonal and adrenal support
- Individualized options for Lyme and/or co-infection treatment
- Solutions for treating CIRS and/or MCAS
- Emotional healing and brain retraining modalities to heal your nervous system
Functional Medicine is Evidence-Based
Research indicates that it takes approximately 15-17 years to translate emerging scientific research into clinical practice, but as healthcare costs become increasingly unsustainable, we don’t have that kind of time. Functional medicine practitioners dramatically reduce that gap by using solid scientific foundations to translate new scientific research findings into clinical practice much more quickly. Functional medicine practitioners are typically early adopters of innovative knowledge and practices because we strive to offer our patients the very best in testing and treatment.
Excitingly, change is coming to mainstream medicine. In 2014, the Cleveland Clinic opened the Center for Functional Medicine, the first functional medicine clinic to exist within an academic medical center in the U.S. The Center is working to transform healthcare using an innovative model of care that shifts the traditional disease-centered focus of medical practice to a more patient-centered approach.
The Center is committed to doing quality, rigorous research that evaluates the impact of the functional medicine model of care on patient outcomes. Current research includes investigations of the model of care and targeted interventions for specific chronic conditions.
At CCFM, we believe that science and technology are our allies, and are powerful forces that must simultaneously be married to evolutionary knowledge respecting the ancient needs of our body, mind, and soul.
-
- About chronic diseases. The Centers for Disease Control and Prevention. https://www.cdc.gov/chronicdisease/about/index.htm. Published October 23, 2019. Accessed September 9, 2020.
- Beidelschies M, et al. Association of the functional medicine model of care with patient-reported health-related quality-of-life outcomes. JAMA. 2019; 2(10): e1914017.
- Vighi G, et al. Allergy and the gastrointestinal system. Clin Exp Immunol. 2008; 153(Suppl 1): 3-6.
- Wilkins LJ, et al. Defining dysbiosis for a cluster of chronic diseases. Sci Rep. 2019; 9: 12918.
- Mu Q, et al. Leaky gut as a danger signal for autoimmune diseases. Front Immunol. 2017; 8: 598.
- Blander JM, et al. Revisiting the old link between infection and autoimmune disease with commensals and T helper 17 cells. Immunol Res. 2012; 54(1-3): 50-68.
- The Sonnenburg lab: The gut microbiota. Stanford University website. https://sonnenburglab.stanford.edu/research.html. Accessed September 11, 2020.
- Furman D, et al. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019; 25(12): 1822-1832.
- Thompson PA, et al. Environmental immune disruptors, inflammation and cancer risk. Carcinogenesis. 2015; 36(Suppl 1): S232-S253.
- Diamanti-Kandarakis E, et al. Endocrine-disrupting chemicals: An Endocrine Society scientific statement. Endocr Rev. 2009; 30(4): 293-342.
- Tu P, et al. Gut microbiome toxicity: Connecting the environment and gut microbiome-associated diseases. Toxics. 2020; 8(1): 19.
- Marsit CJ, et al. Influence of environmental exposure on human epigenetic regulation. J Exp Biol. 2015; 218(1): 71-79.
- McEwan BS. Stressed or stressed out: What is the difference? J Psychiatry Neurosci. 2005; 30(5): 315-318.
- Tai-Seale M, et al. Time allocation in primary care office visits. Health Serv Res. 2007; 42(5): 1871-1894.


